Osteoporosis
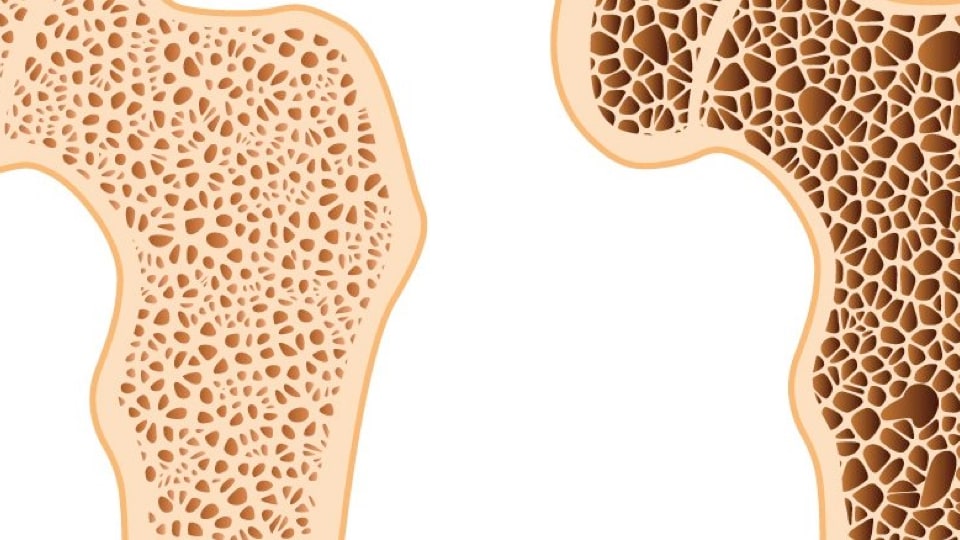
Osteoporosis is a progressive metabolic bone disease that results in increased bone fragility and fracture tendency as a result of low bone mass and deterioration of the microarchitecture of bone tissue.
With the prolongation of human life and the increase in the aging population all over the world, it has become an increasingly important health problem. It is estimated that more than 200 million people today are osteoporotic.
The society in Turkey is getting older and therefore osteoporosis stands out as an important health problem. Osteoporosis is also a disease that creates a risk of fracture. The most important complication of the disease is bone fractures, which can cause many secondary health problems and even be fatal.
Bone is a very dynamic organ; It is constantly lost (resorption) and rebuilt (formation). Bone mass forms and grows (modeling) from birth to adolescence.
Although peak bone mass is determined mainly by genetic factors, it is closely related to gender, nutrition, physical activity and health during growth. While it is maintained at the same level in the 20-30s, losses begin later, with menopause in women and aging in both sexes. Bone loss gradually increases.
The most important clinical consequence of osteoporosis is fragility fractures. Fragility fractures are fractures that occur as a result of mechanical forces known as low-level, low-energy trauma that would not normally cause a fracture.
Osteoporosis Diagnosis Methods
Recommended for the diagnosis of osteoporosis is the measurement of BMD by the dual X-ray absorptiometry (DXA) method.
Measuring the patient's height is also a practical method for osteoporosis risk assessment. It is also an important finding that during the examination, the patient's height is 4.0 cm less than the height he knew when he was young (20 years old) or 1.5-2 cm less than the height recorded in the previous examination.
Osteoporosis Risk Factors
Inactivity
Insufficient physical activity is the most important risk factor for osteoporosis. This also applies to bedridden young people. These patients lose approximately 30% of their bone mass within a few months, and it may take years to regain baseline levels. For this reason, rest periods during illnesses should be kept as short as possible.
Extreme Sports
Continuous and strenuous work, extreme dieting, and strict control of body weight can lead to an excessive decrease in body fat and decreases in estrogen levels in women, which can increase the risk of fractures.
Extreme Weakness
The risk of fracture is high in thin women. Weight gain causes bones to become stronger and estrogen metabolites produced by fat cells protect bones from osteoporosis. Excessive weakness causes osteoporosis; Excessive weight gain may also cause undesirable conditions such as deterioration of the vertebrae, wear and tear in the knee and ankle joints, and arthritis.
Smoking
Smoking doubles the risk of osteoporosis. For 1 pack of cigarettes per day during adulthood, women's bone mineral density at menopause is 5-10% lower than non-smokers. Smoking increases the lifetime risk of spinal fractures by 13-32% in women and men. The risk of hip fracture increases by 30-40%. Smoking reduces the activation of vitamin D by increasing blood cortisone levels. It affects estrogen metabolism in the liver and increases its destruction. It causes deficiency of some vitamins such as vitamin C, which is necessary for bone formation in the body.
Alcohol Intake
Alcohol reduces bone formation by affecting the hormones that regulate calcium and paves the way for osteoporosis. In excessive alcohol consumption, calcium absorption decreases and its excretion increases. The determining factors here are malnutrition accompanying alcohol, low body weight, liver damage, decreased calcium absorption, and decreased estrogen levels.
Excess Caffeine Consumption
It negatively affects bone health by reducing calcium absorption and causing hypercalciuria.
Presence of Concomitant Disease
Cardiovascular diseases, diabetes, hyperthyroidism and connective tissue diseases, rheumatic diseases, stomach and intestinal malabsorption disrupt bone mineralization and have a negative impact on hip bone mineral density, especially.
Drugs Used
Corticosteroids, antiepileptics, diuretics, anti-depressant drugs, lithium, methotraxate, proton pump inhibitors (stomach protectors) and anticoagulant drugs.
Hormonal Causes
Decrease in estrogen due to menopause in women, low testosterone in men, hyperthyroidism, hyperparathyroidism, Cushing's disease.
Stress
It accelerates bone destruction by increasing endogenous cortisol production, reduces bone formation, and weakens bones by reducing the absorption of calcium from the intestine. Chronic stress activates the HPA axis and sympathetic nervous system, suppresses the secretion of reproductive hormone and growth hormone, and causes tissue damage.It causes bone loss by increasing the inflammatory secretions of cells, ultimately preventing bone formation and stimulating bone destruction.
Calcium Deficiency
If dietary calcium intake is not sufficient during growth, skeletal construction cannot reach its peak. When calcium intake is low over the years, the release of parathormone stimulates the removal of calcium from bone stores and, as a result, osteoporosis may develop. The more calcium intake is during childhood and adolescence, the better the peak bone mass will be, and the risk of fractures that will occur with aging in men and women will be reduced. Although milk and dairy products are the most common sources of calcium, many products such as dark green leafy vegetables and oilseeds have high calcium content.
Calcium content per 100 grams of food;
|
Nutrition |
mg |
|
Kashar Cheese |
700 |
|
Okra (dried) |
678 |
|
Green Beans |
480 |
|
Molasses (Grapes) |
400 |
|
Vine Leaf |
392 |
|
Mallow |
249 |
|
Almond |
234 |
|
Soybeans |
226 |
|
Hazelnut |
209 |
|
Arugula |
205 |
|
Parsley |
203 |
|
Mint (Fresh) |
200 |
|
Madımak |
166 |
|
White Cheese (Fat) |
162 |
|
Dried Beans |
144 |
|
Eggplant |
137 |
|
Kullet beans |
135 |
|
Pistachios |
131 |
|
Cow's Milk (Skimmed) |
123 |
|
Sunflower Seeds |
120 |
|
Yogurt (Full Fat) |
120 |
|
Pepper (dried) |
120 |
|
Cow's Milk (Full Fat) |
119 |
|
Black Cabbage |
116 |
|
Biceps |
114 |
|
Sesame |
110 |
|
Kiwi |
100 |
|
Walnut |
99 |
|
Feta Cheese (Fat-Free) |
96 |
|
Spinach |
93 |
Vitamin D Deficiency
Our bones need calcium, vitamin D and many other elements. Having these elements in balance is as important as whether they are taken or not. Today, vitamin D is a vitamin that plays a role in all metabolic events, from cancer to immunity, from osteoporosis to multiple sclerosis, cardiovascular diseases and diabetes, and its importance is increasingly understood. Vitamin D increases the absorption of calcium and ensures proper regeneration and mineralization of bone. It reduces the risk of falling as it has a stimulating effect on the muscle. Calcium taken without added vitamin D may cause calcium deposits in soft tissues and vessels. Therefore, if calcium is taken together with vitamin D, there is no need for high doses of calcium. It is reported that when the blood level of vitamin D exceeds 30ng / dl, there is a decrease in the risk of cancer, autoimmune diseases, Type 2 diabetes, Type 1 diabetes cardiovascular disease, infection risks and a decrease in the risk of death from all diseases.
Vitamin K2 Deficiency
Vitamin K2 is synthesized mainly by bacteria. It goes to blood vessels and bones. It prevents precipitation, especially in the vascular wall, during calcium intake. Its role is to help transport calcium to appropriate areas in our body, such as our bones and teeth.
Vitamin K2 plays a role in regulating the bone quality enhancing function of osteocalcin. By enabling osteocalcin to be activated by gamma carboxylation, calcium is released into bone hydroxyapatite.It connects to . Vitamin K2 is involved in the modulation of the nuclear receptor activator factor -kb- ligand by inhibiting RANKL, the main pathway regulating osteoclastic activity, and reducing osteoclastogenesis. Other data suggest that vitamin K2 increases osteoblastogenesis via the steroid and xenobiotic receptor (SRX), a nuclear receptor called osteoblasts that promotes collagen deposition.
Low vitamin K2 intake is often associated with skeletal fragility. A prospective study shows that vitamin K insufficiency increases the risk of hip fracture in women aged 38-63.
Magnesium Deficiency
For bone health, calcium / magnesium balance is more important than increasing calcium intake. Magnesium is a mineral that every cell in our body needs. Half of the magnesium stores are found in the cells of tissues and organs, the other half is found in the bone together with calcium and phosphate, and only 1% is found free in the blood. Keeping the magnesium level in the blood constant is important for maintaining functions. Magnesium must exist in a certain balance with calcium in the body. If the balance between magnesium and calcium is not maintained, excess calcium becomes toxic to the body and causes heart disease, arrhythmias, arthritis, osteoporosis, arteriosclerosis, calcification of tissues and organs. Magnesium takes part as a co-factor in many biochemical reactions, helps maintain normal muscle and nerve function, maintain heart rhythm and maintain bone strength.
Boron Deficiency
Deficiency can be prevented by including boron-rich foods such as prunes, avocados, black grapes, peanuts, apples and broccoli in our diet.
Molybdenum Deficiency
It is important to have a diet rich in foods with high molybdenum content, such as black-eyed peas, beans, green leafy vegetables, meat and eggs.
Strontium Deficiency
Important strontium sources such as seafood, meat, poultry, and root vegetables should definitely be included in our diet.
Dysbiosis
Recent studies show that the microbiome may have an impact on bone remodeling and bone mass. Probiotic treatment has been shown to reduce bone loss in estrogen-deficient animals.
Prebiotics are non-digestible carbohydrate compounds that, when consumed, provide health benefits and help prevent and treat chronic diseases. While prebiotics are known to improve a number of chronic, inflammatory conditions, there is also increasing evidence showing their effects on calcium metabolism and bone health.
Prebiotics reportedly increase calcium absorption and improve measurements of bone mineral density and strength in rodent models. Data from growing children and postmenopausal women indicate that prebiotics have both short- and long-term effects that beneficially influence bone turnover and mineral deposition in the skeleton. It suggests that fiber diets may be a suitable and effective method for maximizing mineral deposition in growing children and preventing bone loss in later years, when osteoporosis is a greater risk.
Sodium / Potassium Balance Disorder
While the human species evolved to have potassium intake 4-10 times the sodium intake, today this ratio has reversed to sodium intake 3-10 times the potassium intake. As it stands, we are the only mammal species in nature that consumes more sodium than potassium. The sodium/potassium ratio is a more important criterion than sodium intake in hypertension. Sodium intake also increases urinary calcium excretion, so in the case of osteoporosis, excessive salt intake should be given more attention than dietary calcium intake deserves. Increasing dietary potassium bicarbonate intake reduces urinary calcium excretion caused by excessive salt (sodium) intake, thus contributing to the prevention of osteoporosis. Packaged foods disrupt the sodium / potassium balance:
The first thing to do to regulate the sodium potassium balance is; It is to exclude packaged foods containing large amounts of salt from the diet. Emphasizing that potassium support is a key role, let's say that all plants are rich in potassium and poor in salt. For example, the potassium / sodium ratio is 220 in walnuts, 75 in mushrooms, 70 in avocados, 705 in almonds, 10 in parsley and 10 in kale. Plant foods contribute to our health with both the phytonutrients they contain and the alkaline salts they contain.
Tissue Acidosis
A diet rich in packaged, processed foods, unhealthy fats and sugar keeps our body in a metabolic acidosis that lasts for years without any symptoms. This tissue acidosis both increases calcium withdrawal from bone and reduces bone formation and promotes its destruction. FToo little protein intake also contributes to osteoporosis because it causes acidosis. As in everything else, balance is essential in protein intake. In other words, just like taking too much protein, taking too little protein weakens the bone structure.
What Do We Do From a Functional Perspective in Osteoporosis Prevention and Treatment?
As with all chronic diseases, we start with the intestines and repair leaky gut if there is any, and educate our patients about healthy nutrition and lifestyle changes.
Our Main Principles in Nutrition:
- Staying away from packaged foods, including colorful vegetables, healthy oils and oilseeds in the diet,
- Supplementing vitamin and mineral deficiencies with a balanced diet and supplements when necessary (When it comes to osteoporosis, we now know that not only calcium and vitamin D are important, but also magnesium, k2, boron, molybdenum and strontium).
- Reducing salt intake, increasing potassium intake
- Avoiding latent acidosis by maintaining the balance between proteins and vegetables and focusing on plant proteins instead of animal proteins
- Paying attention to micronutrient intake and the balance between them
Lifestyle Changes
- Finding appropriate methods for the patient to control stress,
- Ensuring sleep hygiene,
- Exercise regulation: Exercise is effective in preserving bone mass. Regular weight-bearing and muscle-strengthening exercise is recommended. Exercises performed against gravity are defined as weight-bearing exercises. In addition to walking, activities such as dancing, stair climbing, jumping, weight lifting and tennis can be done as weight-bearing exercises. Muscle strengthening exercises include balance, resistance and posture exercises such as yoga and pilates. Since swimming is not done against gravity, swimming does not have a positive effect on bones.
- Providing bio-equivalent hormone replacement when necessary to ensure hormone balance,
- Replacement of missing vitamins and minerals
Bibliography
ATASOY, D. M. (2018). Functional Medicine. Istanbul: US Academy.
CAPOZZI, A., SCAMBIA, G., & LELLO, S. (2020). Calcium, vitamin D, vitamin K2, and magnesium supplementation and skeletal health. Maturitas , 55-63.
DE NIJS, R. N. (2008). Glucocorticoid-induced osteoporosis: a review on pathophysiology and treatment options. Minerva Med. , 23-43.
KÜHN, J., TROTZ, P., & STANGL, G. (2018). Prevalence of vitamin D insufficiency and evidence for disease prevention in the older population. Springer , 1-6.
SAYGILI, P. D. (2020). Osteoporosis and Metabolic Bone Diseases Diagnosis and Treatment Guide. Ankara: TURKISH ENDOCRINOLOGY and METABOLISM SOCIETY.
VAN DE BERGH, J. P., BOURS, S. P., VAN GEELl, T. A., & GEUSENS, P. P. (2010). Optimal Use of Vitamin D When Treating Osteoporosis. Springer , 36-42.
WHISNER, C. M., & CASTILLO, L. F. (2017). Prebiotics, Bone and Mineral Metabolism. Springer , 1-37.
